ADME DEFINITION:
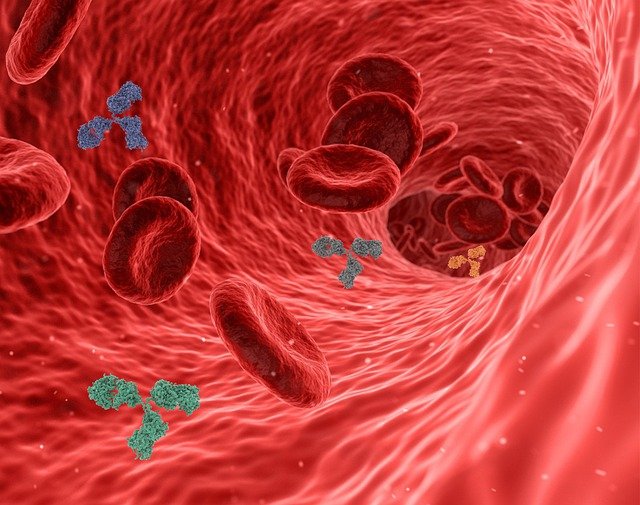
Absorption, distribution, metabolism, and excretion are sometimes referred to collectively as ADME processes. These processes determine when the drug appears in the blood stream and for how long it remains in the blood stream to give noticeable action.
-
Absorption, distribution, metabolism, and excretion
-
When & how long the drug appears in the blood stream
-
therapeutic response is dependent upon the ADME processes
In order for a drug to cause a therapeutic response, it must reach adequate concentrations in the blood so that it can reach and interact with drug receptors in adequate numbers to trigger a noticeable action. The course of drug action is, therefore, directly correlated with the concentration of the drug in the blood stream, and is dependent upon the ADME processes.
ABSORPTION:
Absorption is the transfer of a drug from its site of administration to the bloodstream. The rate and extent of absorption depends on the route of administration, the formulation and chemical properties of the drug, and physiologic factors that can impact the site of absorption.
-
Transfer of a drug from site to the blood
-
route of administration, Drug properties
-
IV route is fastest and effective for ABSORPTION
-
Highly water-soluble drugs absorb more readily than fat-soluble drugs
-
Drugs with smaller particle sizes ABSORB easily
When a drug is administered intravenously, absorption is not required because the drug is transferred from the administration device directly into the bloodstream. In the case of intravenous administration, the entire dose of the drug is available to move to the sites of drug action. Administration by other routes may result in less availability due to incomplete absorption. When this occurs, less of the drug is delivered by the bloodstream to the site of action. When a tablet or capsule is swallowed it must dissolve before it can be absorbed. The dissolving of a tablet or capsule is referred to as dissolution. Manufacturing processes and the water solubility of the drug affect dissolution rates. Highly water-soluble medications dissolve more readily in the gastrointestinal (GI) tract, while fat-soluble drugs dissolve more slowly. Drugs with smaller particle sizes go into solution more readily. The inert ingredients added to formulations can also affect their dissolution
DISTRIBUTION
Distribution is a process when a drug is absorbed into the bloodstream it can be carried throughout the body. This process specifically carrying is called distribution. It is a reversible process; while some molecules may be interacting with receptors on cell membranes or inside of cells, other molecules may move back into the bloodstream.
-
Process of distribution of a drug from the bloodstream to the site of absorption.
-
Factors influencing distribution are blood flow, capillary permeability, the degree of binding and its solubility.
-
Blood-brain barrier protects the brain from entering high concentrations of drugs to CNS central nervous system.
The delivery of a drug from the bloodstream to the site of drug action primarily depends on blood flow, capillary permeability, the degree of binding (attachment) of the drug to blood and tissue proteins, and the relative lipid-solubility of the drug molecule. Blood flow to different organs of the body is not equal. The most vitally important organs of the body receive the greatest supply of blood. These organs include the brain, liver, and kidneys. Skeletal muscle and bone receive less blood, and adipose tissue (fat) receives the least. If blood flow were the only factor affecting distribution, it would be reasonable to expect that high concentrations of administered medications would always appear in the brain and liver. In reality, few drugs exhibit good penetration of the central nervous system. The anatomical structure of the capillary network in the brain creates a significant barrier to the passage of many drugs and is commonly referred to as the blood-brain barrier. This barrier is an adaptation that for the most part protects brain tissue from invasion by foreign substances. To readily penetrate into the brain, drugs must be fairly small and lipidsoluble or must be picked up by the carrier-mediated transport mechanism in the central nervous system. This explains why the small and highly fat-soluble anesthetic gases quickly and easily penetrate the brain to cause anesthesia, while other larger and water soluble molecules like penicillin antibiotics penetrate the central nervous system to a much lesser degree.
METABOLISM
Drugs are eliminated from the body either unchanged through the kidneys and bile, or they may undergo chemical changes that allow them to be more easily excreted. The process of undergoing chemical changes is called biotransformation, or metabolism. As previously noted, anything absorbed through the GI tract goes directly into the portal circulaextracellular Outside of the cell or cells. interstitial Situated within or between parts of a particular organ or tissue. intracellular Existing or functioning inside a cell or cells. hydrophilic Having an affinity for, readily absorbing, or mixing with water. lipophilic Having an affinity for, or ability to absorb or dissolve in, fats. biotransformation Chemical alterations of a compound that occur within the body, as in drug metabolism. prodrug An inactive drug precursor that is converted in the body to the active drug form. Absorption that feeds into the liver. The liver is adapted to clear toxins from the body and is the major site for drug metabolism, but specific drugs may undergo biotransformation in other tissues. The kidneys cannot efficiently excrete highly fat-soluble drugs that readily cross cell membranes because they are reabsorbed in the last stages of filtration. These compounds must first be metabolized in the liver to more water-soluble compounds and then removed. There are two types of metabolic processes drugs undergo in the liver. Most undergo one or both types of reactions. In the first type of reaction drugs are made more polar through oxidation-reduction reactions or hydrolysis. These reactions use metabolic enzymes, most often those of the cytochrome P450 enzyme system, to catalyze the biotransformation.
-
Metabolism is the process of undergoing chemical changes to get excreted easily is called metabolism
-
Biotransformation is also known as metabolism
-
Major site for drug metabolism is liver and Kidney
-
two types of metabolic processes
-
hydrolysis an enzyme-catalyzed reactions
-
conjugation reactions with glucuronic acid, sulfuric acid, acetic acid, or an amino acid like Glucuronidation.
-
Metabolism converts the prodrug to the active form. Example: Fosphenytoin is a prodrug of phenytoin,
In enzyme-catalyzed reactions, the rate of the reaction is accelerated by the presence of enzymes. A limited amount of enzyme is present at any given time in the liver. Since the rate of enzyme-catalyzed drug metabolism is limited by the quantity of available enzyme, metabolism in these cases is considered a saturable process. This means that the rate of conversion will only continue at the normal pace until the available supply of enzyme is used. At that point, metabolism is slowed until enzyme becomes available again. For the usual doses of most drugs, these reactions never reach saturation. There are a few drugs where doses may reach the saturation point of the enzymes. Once enzymes become saturated, blood levels increase exponentially toward toxicity. Examples include metabolism of alcohol and phenytoin. The second type of metabolism involves conjugation reactions. In this type of reaction the drug undergoing change is joined with another substance, such as glucuronic acid, sulfuric acid, acetic acid, or an amino acid. Glucuronidation is the most common conjugation reaction. The result of conjugation is a more water-soluble compound that is easier for the kidneys to excrete. These metabolites are most often therapeutically inactive. Some agents are initially administered as an inactive compound (prodrug) in order to improve availability or reduce side effects. Metabolism converts the prodrug to the active form. Fosphenytoin, for example, is a prodrug of phenytoin, a drug used for seizure disorders. Fosphenytoin is more completely and quickly absorbed when given by IM injection than phenytoin and can be used in critical situations with greater ease because it dose not require insertion of an intravenous catheter.
EXCRETION
When a drug is taken into and distributed throughout the body, it must be subsequently removed, or concentrations of the drug would continue to rise with each successive dose. The complete removal of the drug from the body is referred to as elimination. Elimination of the drug encompasses both the metabolism of the drug, and excretion of the drug through the kidneys, and to a much lesser degree into the bile. Excretion into the urine is one of the most important mechanisms of drug removal. The kidneys act as a filter for the blood and create urine as a vehicle for removal of waste. Blood enters the kidney through renal arteries and then is filtered by the glomerulus.
-
The complete removal of the drug from the body is referred to as elimination.
-
Excretion of the drug through the kidneys into the urine is one of the most important mechanisms of drug removal aside of liver.
-
the amount being taken in by the patient is equal to the amount being removed by the liver and kidneys. This state of equilibrium is called steady state
The glomerular filtrate becomes concentrated and substances are removed as it passes through the renal tubule and eventually becomes urine. Drug molecules in the bloodstream that are not bound to albumin are also filtered out into the glomerular filtrate. When drugs have not been converted to water soluble compounds in the liver, they are likely to be reabsorbed back into the bloodstream at the end of the filtration process, and will cycle through the body again. If they are water soluble, they will end up in the urine and be excreted. When a medication is given repeatedly, as most are in real patients, the total amount of drug in the body will increase up to a point and then stabilize. At this point, the amount being taken in by the patient is equal to the amount being removed by the liver and kidneys (Fig. 3.7). This state of equilibrium is called steady state, and drug levels will remain fairly constant unless there is a dose change, an interruption in treatment, or failure of the organs of elimination. The therapeutic effects of many drugs are closely correlated to a specific range of steady state serum drug levels, and physicians or clinical pharmacists will monitor these levels and adjust doses when necessary so that patients obtain the appropriate drug response.