ROUTES OF DRUG ADMINISTRATION: The possible routes for drug entry into the body. Most drugs can be administered by a variety of routes. The choice of appropriate route in a given situation depends both on drug as well as patient related factors. Mostly common sense considerations, feasibility and convenience dictate the route to be used. Generally routes of drug administration refer to the right path or the required route through which a drug has to be administered into the body to obtain maximum benefit. Here is the list of 5, 10+ outes of drug administration.
- oral
- sublingual
- rectal
- nasal
- ocular
- otic
- inhalation
- nebulization
- transdermal
- Subcutaneous (under the skin)
- Intramuscular (in a muscle)
- Intravenous (in a vein)
- Intrathecal (around the spinal cord
Factors governing choice of route
- Physical and chemical properties of the drug (solid/ liquid/gas; solubility, stability, pH, irritancy).
- Site of desired action—localized and approachable or generalized and not approachable.
- Rate and extent of absorption of the drug from different routes.
- Effect of digestive juices and first pass metabolism on the drug.
- Rapidity with which the response is desired (routine treatment or emergency).
- Accuracy of dosage required (i.v. and inhalational can provide fine tuning).
- Condition of the patient (unconscious, vomiting).
Routes of Administration can be broadly divided into those for
(a) Local action and (b) Systemic action.
LOCAL ROUTES
These routes can only be used for localized lesions at accessible sites and for drugs whose systemic absorption from these sites is minimal or absent. Thus, high concentrations are attained at the desired site without exposing the rest of the body. Systemic side effects or toxicity are consequently absent or minimal. For drugs (in suitable dosage forms) that are absorbed from these sites/routes, the same can serve as systemic route of administration, e.g. glyceryl trinitrate (GTN) applied on the skin as ointment or transdermal patch. The local routes are:
-
Topical
This refers to external application of the drug to the surface for localized action. It is often more convenient as well as encouraging to the patient. Drugs can be efficiently delivered to the localized lesions on skin, oropharyngeal/ nasal mucosa, eyes, ear canal, anal canal or vagina in the form of lotion, ointment, cream, powder, rinse, paints, drops, spray, lozengens, suppositories or pesseries. Nonabsorbable drugs given orally for action on g.i. mucosa (sucralfate, vancomycin), inhalation of drugs for action on bronchi (salbutamol, cromolyn sodium) and irrigating solutions/jellys (povidone iodine, lidocaine) applied to urethra are other forms of topical medication.
-
Deeper tissues
Certain deep areas can be approached by using a syringe and needle, but the drug should be in such a form that systemic absorption is slow, e.g. intra-articular injection (hydrocortisone acetate in knee joint), infiltration around a nerve or intrathecal injection (lidocaine), retrobulbar injection (hydrocortisone acetate behind the eyeball).
-
Arterial supply
Close intra-arterial injection is used for contrast media in angiography; anticancer drugs can be infused in femoral or brachial artery to localise the effect for limb malignancies.
SYSTEMIC ROUTES
The drug administered through systemic routes is intended to be absorbed into the blood streamand distributed all over, including the site of action, through circulation
-
Oral
Oral ingestion is the oldest and commonest mode of drug administration. It is safer, more convenient, does not need assistance, noninvasive, often painless, the medicament need not be sterile and so is cheaper. Both solid dosage forms (powders, tablets, capsules, spansules, dragees, moulded tablets, gastrointestinal therapeutic systems— GITs) and liquid dosage forms (elixirs, syrups, emulsions, mixtures) can be given orally.
Limitations of oral route of administration
- Action of drugs is slower and thus not suitable for emergencies.
- Unpalatable drugs (chloramphenicol) are difficult to administer; drug may be filled in capsules to circumvent this.
- May cause nausea and vomiting (emetine).
- Cannot be used for uncooperative/unconscious/ vomiting patient.
- Absorption of drugs may be variable and erratic; certain drugs are not absorbed (streptomycin).
- Others are destroyed by digestive juices (penicillin G, insulin) or in liver (GTN, testosterone, lidocaine).
-
Sublingual (s.l.) or buccal
The tablet or pellet containing the drug is placed under the tongue or crushed in the mouth and spread over the buccal mucosa. Only lipid soluble and non-irritating drugs can be so administered. Absorption is relatively rapid—action can be produced in minutes. Though it is somewhat inconvenient, one can spit the drug after the desired effect has been obtained. The chief advantage is that liver is bypassed and drugs with high first pass metabolism can be absorbed directly into systemic circulation. Drugs given sublingually are—GTN, buprenorphine, desamino-oxytocin.
-
Rectal
Certain irritant and unpleasant drugs can be put into rectum as suppositories or retention enema for systemic effect. This route can also be used when the patient is having recurrent vomiting or is unconscious. However, it is rather inconvenient and embarrassing; absorption is slower, irregular and often unpredictable, though diazepam solution and paracetamol suppository are rapidly and dependably absorbed from the rectum in children. Drug absorbed into external haemorrhoidal veins (about 50%) bypasses liver, but not that absorbed into internal haemorrhoidal veins. Rectal inflammation can result from irritant drugs. Diazepam, indomethacin, paracetamol, ergotamine and few other drugs are some times given rectally.
-
Cutaneous
Highly lipid soluble drugs can be applied over the skin for slow and prolonged absorption. The liver is also bypassed. The drug can be incorporated in an ointment and applied over specified area of skin. Absorption of the drug can be enhanced by rubbing the preparation, by using an oily base and by an occlusive dressing.
Transdermal therapeutic systems (TTS)
These are devices in the form of adhesive patches of various shapes and sizes (5–20 cm2) which deliver the contained drug at a constant rate into systemic circulation via the stratum corneum (Fig. 1.2). The drug (in solution or bound to a polymer) is held in a reservoir between an occlusive backing film and a rate controlling micropore membrane, the under surface of which is smeared with an adhesive impregnated with priming dose of the drug. The adhesive layer is protected by another film that is to be peeled off just before application. The drug is delivered at the skin surface by diffusion for percutaneous absorption into circulation. The micropore membrane is such that rate of drug delivery to skin surface is less than the slowest rate of absorption from the skin. This offsets any variation in the rate of absorption according to the properties of different sites. As such, the drug is delivered at a constant and predictable rate irrespective of site of application. Usually chest, abdomen, upper arm, lower back, buttock or mastoid region are utilized. Transdermal patches of GTN, fentanyl, nicotine and estradiol are available in India, while those of isosorbide dinitrate, hyoscine, and clonidine are marketed elsewhere. For different drugs, TTS have been designed to last for 1–3 days. Though more expensive, they provide smooth plasma concentrations of the drug without fluctuations; minimize interindividual variations (drug is subjected to little first pass metabolism) and side effects. They are also more convenient— many patients prefer transdermal patches to oral tablets of the same drug; patient compliance is better. Local irritation and erythema occurs in some, but is generally mild; can be minimized by changing the site of application each time by rotation. Discontinuation has been necessary in 2–7% cases.
-
Inhalation
Volatile liquids and gases are given by inhalation for systemic action, e.g. general anaesthetics. Absorption takes place from the vast surface of alveoli—action is very rapid. When administration is discontinued the drug diffuses back and is rapidly eliminated in expired air. Thus, controlled administration is possible with moment to moment adjustment. Irritant vapours (ether) cause inflammation of respiratory tract and increase secretion.
-
Nasal
The mucous membrane of the nose can readily absorb many drugs; digestive juices and liver are bypassed. However, only certain drugs like GnRH agonists and desmopressin applied as a spray or nebulized solution have been used by this route. This route is being tried for some other peptide drugs like insulin, as well as to bypass the bloodbrain barrier.
-
Parenteral
Conventionally, parenteral refers to administration by injection which takes the drug directly into the tissue fluid or blood without having to cross the enteral mucosa. The limitations of oral administration are circumvented. Drug action is faster and surer (valuable in emergencies). Gastric irritation and vomiting are not provoked. Parenteral routes can be employed even in unconscious, uncooperative or vomiting patient. There are no chances of interference by food or digestive juices. Liver is bypassed. Disadvantages of parenteral routes are—the preparation has to be sterilized and is costlier, the technique is invasive and painful, assistance of another person is mostly needed (though self injection is possible, e.g. insulin by diabetics), there are chances of local tissue injury and, in general, parenteral route is more risky than oral.
The important parenteral routes are:
(i) Subcutaneous (s.c.)
The drug is deposited in the loose subcutaneous tissue which is richly supplied by nerves (irritant drugs cannot be injected) but is less vascular (absorption is slower than intramuscular). Only small volumes can be injected s.c. Self-injection is possible because deep penetration is not needed. This route should be avoided in shock patients who are vasoconstricted— absorption will be delayed. Repository (depot) preparations that are aqueous suspensions can be injected for prolonged action. Some special forms of this route are:
(a) Dermojet
In this method needle is not used; a high velocity jet of drug solution is projected from a microfine orifice using a gun like implement. The solution passes through the superficial layers and gets deposited in the subcutaneous tissue. It is essentially painless and suited for mass inoculations.
(b) Pellet implantation
The drug in the form of a solid pellet is introduced with a trochar and cannula. This provides sustained release of the drug over weeks and months, e.g. DOCA, testosterone.
(c) Sialistic (nonbiodegradable) and biodegradable implants
Crystalline drug is packed in tubes or capsules made of suitable materials and implanted under the skin. Slow and uniform leaching of the drug occurs over months providing constant blood levels. The nonbiodegradable implant has to be removed later on but not the biodegradable one. This has been tried for hormones and contraceptives (e.g. NORPLANT).
(ii) Intramuscular (i.m.)
The drug is injected in one of the large skeletal muscles—deltoid, triceps, gluteus maximus, rectus femoris, etc. Muscle is less richly supplied with sensory nerves (mild irritants can be injected) and is more vascular (absorption of drugs in aqueous solution is faster). It is less painful, but self injection is often impracticable because deep penetration is needed. Depot preparations (oily solutions, aqueous suspensions) can be injected by this route. Intramuscular injections should be avoided in anticoagulant treated patients, because it can produce local haematoma.
(iii) Intravenous (i.v
.) The drug is injected as a bolus (Greek: bolos–lump) or infused slowly over hours in one of the superficial veins. The drug reaches directly into the blood stream and effects are produced immediately (great value in emergency). The intima of veins is insensitive and drug gets diluted with blood, therefore, even highly irritant drugs can be injected i.v., but hazards are—thrombophlebitis of the injected vein and necrosis of adjoining tissues if extravasation occurs. These complications can be minimized by diluting the drug or injecting it into a running i.v. line. Only aqueous solutions (not suspensions, because drug particles can cause embolism) are to be injected i.v. and there are no depot preparations for this route. Chances of causing air embolism is another risk. The dose of the drug required is smallest (bioavailability is 100%) and even large volumes can be infused. One big advantage with this route is—in case response is accurately measurable (e.g. BP) and the drug short acting (e.g. sodium nitroprusside), titration of the dose with the response is possible. However, this is the most risky route—vital organs like heart, brain, etc. get exposed to high concentrations of the drug.
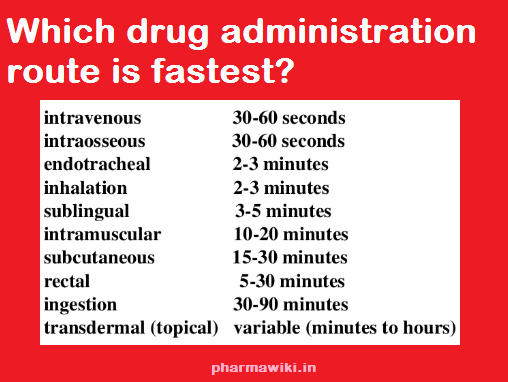
ROUTES OF DRUG ADMINISTRATION 10 Fastest routes
ROUTES OF DRUG ADMINISTRATION 10 Fastest routes PDF
(iv) Intradermal injection
The drug is injected into the skin raising a bleb (e.g. BCG vaccine, sensitivity testing) or scarring/multiple puncture of the epidermis through a drop of the drug is done. This route is employed for specific purposes only.
Search Terms
10 routes of drug administration, routes of drug administration ppt, routes of drug administration pdf, , routes of drug administration in animals, 5 routes of medication administration, assignment on routes of drug administration, parenteral route of drug administration, What are the 5 routes of drug administration?, What are the 6 routes of drug administration?, How are drugs administered?, Which drug administration route is fastest?,