Good Clinical Practice (GCP) Inspection Preparation and Guidance for Clinical Trials Units is a GCP INSPECTION CHECKLIST is here to help registered clinical trial units. This article is for guidance only and is not intended to replace information or advice from the Government. It is always recommended check official site Central Drugs Standard Control Organization for advice and guidance in order to be aware of current guidance.
I. General
Good Clinical Practice (GCP) Inspection General Checklist
- Name and address of the clinical trial site
- Date of Inspection
- Inspection Team Members:
- Personnel present during Inspection (with name and role/designation.)
- Address & Contact details of Investigator:
- Name & address of the Sponsor
- Name & address of clinical trial NOC holder
- Name & address of EC
- Protocol Title
- Protocol Number
Version/date
Protocol amendments, if any. - Investigational Product
- Stage of study:
(Mark the relevant)
(A) Before Trial Commencement
(B) During Conduct of the trial
(C) After Completion of Trial - Type of Inspection:
Surveillance
For Cause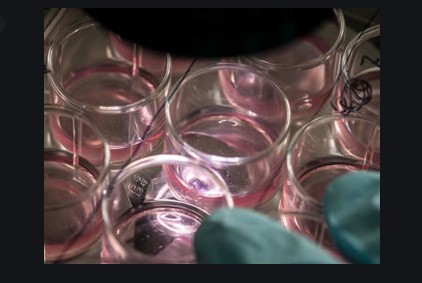
II.LEGAL & ADMINISTRATIVE ASPECTS: GCP checklist
- Clinical trial NOC from O/o DCGI
(Note: mention along with Protocol no., Ver., date) - NOC for subsequent protocol amendments, if any from O/o DCGI
- Ethics Committee approval date
(Note: mention along with Protocol no., Ver., date)
Appendix VII as per Sch.-Y
(mention revision(s) and notification to O/o DCGI, if any) - Whether valid financial agreement between the Sponsor, Investigator & Institution available.
- Whether liability of involved parties (Investigator, Sponsor and Institution) clearly agreed.
- Is the valid clinical trial Insurance available?
- Site Initiation date
- Date of screening of first subject,
- Date of signing ICF by the first subject
- Date of Last Patient-Last Follow-Up (if applicable)
- Whether SOP for various activities are established and documented.
- Verify, whether the hospital/institute/site has adequate emergency care facilities to handle emergency situation.
- Good Clinical Practice (GCP) Inspection Preparation & Guidance for Clinical Trials Units #PPT PDF
III Organisation & Personnel
GCP Inspection Checklist for Organisation & Personnel
- Assure that signed & dated, Curriculum Vitae is available for the Investigator, Sub Investigator /Co-Investigator
- Confirm the educational qualification of the Investigator with registration by Medical Council of State/India.
- Confirm the GCP, Schedule Y and protocol specific training of Investigator, Sub-Investigator/Co-Investigator and its team.
- Determine whether authority for conducting various clinical trial activities were delegated properly by
- Investigator to competent personnel (obtain the list of personnel and duty delegation log).
Check whether the person whom the authority is delegated is adequately qualified and trained for the activity/activities assigned. - Obtain the list of all clinical trials performed by Investigator (Preferably for last three years)
- Ensure that the Investigator is involved in conduct of not more than three clinical trials at a time.
IV Conduct of Trial
GCP Inspection Checklist for Conduct of Trial
A.Screening of subjects:
- Check and review the informed consent for the screening of the subjects.
- Check site screening log & enrolment log and obtain authenticated copy.
- Check whether the subjects are meeting the inclusion/exclusion criteria as per the approved protocol w.r.t review of source documents &/or CRF.
3.1 Clinical Examination by Investigator ( Check patient file/Source documents)
3.2 Verify ,Clinical Laboratory Evaluation( Check Blood Cell Counts, Biochemical test, Urine analysis etc.as required by protocol)
3.3 Verify X-Ray, MRI, ECG, USG or any other technique required to ascertain the inclusion/exclusion criteria.
3.4 Verify, Whether all conditions of Clinical trial NOC are followed or not?
B. Subject record and Informed consent:
- Whether ICF have all the elements enlisted in Appendix V of Schedule Y.
Whether ICF is approved by Ethics Committee prior to consent process. - Whether IC has been obtained from each subject prior to participation of the subject in the study.
- Whether signature/thumb impression of the subjects/legal representative have been affixed with date.
- Whether in case of illiterate subjects or illiterate representative of a subject, there are signature and details of an impartial witness.
- Have witness/ signature being personally dated.( If applicable).
- Have patient/witness signature been personally dated?
- Has the dated signature of the designated person for administering informed consent (IC) been affixed?
- Is the designated person for administering IC medically qualified?
- If IC has been administered by a designated person who is not medically qualified, is there evidence that subject’s queries of a medical nature were answered by a medically qualified person or the investigator?
- Is the completed ICF signed and dated by the investigator?
- Check weather re-consenting is done for changes in ICF, if any.
B.1 Audio-Visual recording of Informed Consent Process( For ‘vulnerable population’ in ‘New Chemical Entities (NCEs) clinical trial’ only & Anti HIV & Anti-Leprosy patients only Audio recording) ( Verify as per GSR 611(E) dated 31.07.2015 )
- Whether audio-visual recording is performed for all subjects, independently.
- Is audio-visual recording conducted in a room conducive to recording of disturbance free audio and video of the consent process?
- Check whether the video recording is free from disturbance to ensure that the image is recognizable and the audio is clearly audible.
- Check whether the recording of informed consent process is preserved safely.
C. Source Documents and Case Record Form
- Verify condition, completeness, legibility, accessibility of the investigators source data file. ( source data includes study subject’s files, recording from automated instruments, tracings, X-ray and other films, laboratory notes, photograph negatives, magnetic media, hospital records, clinical and office charts, subject’s diaries, evaluation checklists and pharmacy dispensing records)
- Whether subject received the test drug with respect to dose and frequency according to the protocol;
- Determine whether safety/ efficacy end point data( Clinical, laboratory examination results) were collected and reported in accordance with the protocol
- Does medical record mentions subject ID/ name /hospital registration number / and indication that subjects are participating in a clinical trial
- Compare the source document with CRF and determine whether source data have been correctly transcribed in CRF;
- Verify the drop-outs and reason for drop-out of subject is appropriately recorded.
- Whether the withdrawal of subject from the study is recorded and appropriately justified in accordance with approved protocol.
- Verify whether Standard Operating Procedure of handling of Serious Adverse Event occurred in clinical trial is available.
- Verify whether all SAE’s have been reported to the sponsor, EC and Licensing authority as per the timelines in accordance with Schedule Y.
(Verify as per GSR 53(E) dated 30.01.2013 & GSR 889 (E) dated 12.12.14 effective from 12.06.2015 ) - Verify Whether SOP for medical care during serious adverse event is available or not.
- Verify whether adequate medical care have been given to the subject especially in the event of inter current illness, adverse events including abnormal lab parameters;
- Verify whether all study related activities are performed at site approved by O/o DCGI.
VI. Sponsor
- all report submitted to the sponsor;
- Whether all CRF were submitted to sponsor after completion of study;
- Determine whether all dropout and reason thereof were reported to sponsor;
- Determine the method and frequency of monitoring the progress of the study by the sponsor and corrective action by site.
- Whether sponsor appointed a monitor with appropriate qualification and experience to monitor trial at the site.
- Whether a log of onsite monitoring visit is maintained at the site.
- Is monitor submits visit report with deviations if any to the sponsor.
- Whether sponsor performed an audit as a part of QA in order to independent and separate from routine monitoring of quality control function.
- In case the investigator and sponsor agrees to prematurely terminate or suspend the study for any reason, whether it was promptly informed to study subjects, Ethics Committee and Licensing Authority.
VII. Investigational Product
GCP Checklist for Investigational Product
- Whether investigator maintain copies of Review individual subject record to verify the correct dose administration with respect to dose, frequency, route of administration
- Determine whether unqualified /unauthorised persons administered/dispensed the test drug
- Determine whether adequate record of quantity of test drug received , dispensed is maintained.( Check the test drug reconciliation and verify the leftover drug or balance on the day of inspection).
- Determine whether storage condition/monitoring method are as per protocol/recommendation;
- Whether trial medication are maintained in secured manner with controlled access
- Have un-used trial medications been returned to the sponsor or disposed of according to protocol?
- Are the drugs dispensing records being maintained properly?
- Whether the records for reconciliation of all IP’s are maintained?
- Are electronic or hand-written temperature logs available for the storage area of the investigational products?
- Verify that investigation product is appropriately labelled. (For clinical trial use only).
VIII. Ethics Committee
GCP INSPECTION CHECKLIST on Ethics Committee
- Identify the name, address of the EC/ IEC in the approval letter and compare it with one stated in Investigator Undertaking.
- Verify the Status of EC-whether Institutional or Independent, Check Registration certificate ( Verify as per GSR 72(E) dated 08.12.2013)
- Verify if EC approval letter mention study code , title and version number of the protocol, list of other documents reviewed, list of members present at the meeting, quorum of five members as specified in Schedule Y satisfied, date, time , venue of the meeting, signature and date of member secretary / Chairman.
Verify whether the EC recorded minutes of meeting. - Verify whether EC is performed on site monitoring of the clinical trial approved.
(Frequency and SOP) - Verify whether EC members have conflict of interest in the approved trial, if yes then the member should abstain from such approval meeting.
- Verify whether the communications between Investigator and EC are available for changes, Serious Adverse Event and deviations occurred in clinical trial.
- Verify whether EC is function in accordance with conditions of registration by LA.
IX Pathology Laboratory ( for Screening/ Assessment)
- Name and address of the clinical laboratory used in the study. (Local and Outside).
- Whether financial & Confidentiality agreement with Investigator and concerned laboratory (ies) in place.
- Is investigator/Sponsor verified the accreditation status and adequacy of the facilities to perform the specified tests as per protocol.
- Verify whether the SOP for sample preparation, handling and transportation is available. Verify the appropriateness of the SOP.
X Quality Assurance
- Verify whether SOP for all procedures conducted at site are available i.e. have a copy of Site Specific and Trial specific SOPs
- Verify the essential components of SOP like who prepared, checked, authorized and when, frequency of SOP revision
- Whether SOPs for all operation like screening and Informed consent Process, AV recording of ICP of vulnerable population in NCE-CTs, SAEs & its Management, Communication with EC/Sponsor/CDSCO, GCP/Sch.Y, training to trial team, training assessment
- Whether SOPs for all operation like IP handling and distribution to study subjects, blood samples collection, processing preservation and transportation to local laboratory.
- Whether SOPs for all operation of storage cabinets, refrigerators/deep freezers used to store samples and IP are available.
- Verify, whether records for job description/responsibilities, qualification and training for all personnel involved in the clinical trial is maintained and stored.
- Verify whether the activities performed are in compliance with duty delegated by Investigator.
- Verify whether concern staff is adequately trained and records maintained there of
- In case of vaccines, are a spillage SOP available and the study team trained to handle such an incidence?
XI Record keeping and data handling
- Is adequate space available for document retention?
- Determine whether documents are maintained properly and for the period as specified.
- Whether necessary measures have been taken to prevent accidental or premature destruction.
- Whether the archival access controlled or restricted to authorized personnel.
- Weather SOP available to document all steps in data management in order to allow step by step retrospective assessment of data quality and study performance.
- Whether corrections in documents carry the date and initials of Investigators and authorized person.
XI-a Electronic data processing
- Is electronic data processing is done by authorized person?
- Verify whether list of authorized persons to make changes is maintained
- Verify if provision for recording of trail of changes and deletions made is available.
- Whether the hardware and software use for data recording and processing is validated
Important NOTE Collect authenticated copies as exhibit wherever any Critical &/or Major non-compliance has been observed.
